- Written by Olivia Alexander
ASCO 2023 roundup: patient-centred communication
The American Society of Clinical Oncology (ASCO) Annual Meeting (June 2–6 2023, Chicago, IL, USA) bought together more than 40,000 oncology professionals from around the world to discuss the central theme, ‘Partnering with patients: the cornerstone of cancer care and research’. We have rounded up some key posters from the meeting where the importance of patient-centred communication in healthcare is highlighted.
What preferences do older cancer patients and their caregivers have when making treatment decisions?
Patients’ decisional control preference can either be:
Older patients are often supported by their doctor or caregiver(s) when making decisions about their treatment. A study looked at decisional control preferences of older patients with cancer and their caregivers, and identified whether opinions were shared by both the patient and caregiver.
They found that the patient and caregiver had a moderate agreement in opinions about the roles that patients and caregivers have in treatment decision-making. Patients (45%) and caregivers (49%) agreed that a decision should be equally shared. The lowest proportion of the pair (2% of patients and 3% of caregivers) agreed that patients should make the decisions by themselves. The highest proportion of both patients (61%) and caregivers (52%) agreed that the patient and caregiver should make the decisions with the doctor’s input.
Knowing what older cancer patients and their caregivers, who often guide treatment decision-making, prefer will guide communication between the healthcare professionals and patients/caregiver(s).
Source: Hryniv S, Gilbride E, Consagra W et al. Exploring decisional control preferences in older patients with cancer and their caregivers. Presented at ASCO 2023 (2–6 June; Chicago, IL, USA).
Do decision-making conversations regarding allogeneic stem cell transplants differ between White and Black patients?
Currently, allogeneic stem cell transplant (alloSCT) is the only treatment that is associated with a cure for high-risk myelodysplastic syndrome (MDS) – a rare type of blood cancer. AlloSCT is a procedure in which a patient receives healthy blood-forming cells (stem cells) from a donor to replace their own stem cells that have been destroyed by cancer treatment.
The possible donors for alloSCT include the patient’s siblings, children and unrelated donors from the international registry. We know that White patients have a much higher chance of finding an unrelated fully matched donor (80%) than Black patients, who only have about a 30% chance.
A study was carried out to see how 37 haematologists, doctors that treat patients with blood and bone marrow disorders, go about discussing donor concerns related to the race of the patient. White and Black actors played the role of the patients in this study.
Overall, conversations with the White patient were reassuring. The haematologists generally assured the patient that they would find a fully matched donor due to there being a high chance of finding one through the international registry.
During conversations with the Black patient, the haematologists emphasized searching for a donor in their family. They also mentioned that with better technology, the option of a half-match with their child was a favourable option. Some haematologists gave the Black patient an overestimation of finding a fully matched donor through the international registry.
Non-White haematologists more often acknowledged the concept of race in stem cell donation, however, overall the haematologists appeared to avoid discussing the lower odds for Black patients to not minimise their hope.
The authors of this study state that these observations will be used to design a prototype communication tool as guidance for haematologists discussing the complex transplant process for high-risk patients.
Rodenbach R, Thordardottir TH & Campbell TC. Will we have a match? Observations from decision making conversations between hematologists and White and Black patients considering allogeneic stem cell transplant. Presented at ASCO 2023 (2–6 June; Chicago, IL, USA).
Do future innovations that are being developed influence treatment recommendations?
A survey of 200 oncologists, doctors that treat cancer, was carried out to find out how expectations of future innovations may influence the treatment recommendations that they may give patients now.
The survey gave different scenarios where a new innovation had either a modest level of effectiveness or one which resulted in a ‘breakthrough’. They were also given a time of arrival, when the innovation would be available, they then asked the oncologists about the likelihood that they would discuss these innovations with the patient and how it would influence their recommended treatment for the patient today.
They found that having a ‘breakthrough’ expected effectiveness and a shorter time to arrival was associated with a significantly greater likelihood of discussing future innovations with patients. The results suggest that it is important that patients understand what future innovations are available to them, whether they are approved or not and the potential risks that come with them so that both the doctor and patient can outweigh the potential risks of current treatment and make effective shared decisions about their treatment.
Source: Li M, Elsisi Z, Wong WB, Kowal S, Veenstra DL & Garrison LP. Do future innovations in development influence oncologists’ treatment recommendations today? Presented at ASCO 2023 (2–6 June; Chicago, IL, USA).
How different can patient-reported symptoms be from clinician-reported symptoms?
Adverse events, undesired effects of a drug or other type of treatment, reported by clinicians are usually what determines how safe a new medication is, however, patient-reported outcomes (PROs) may better represent the treatment’s impact on overall patient functioning and wellbeing. Information from a study called POLARIX was evaluated to see how PRO symptoms compare to clinician-reported adverse events.
The severity of the adverse events was also reported. They found that, overall, patients reported a higher incidence and severity of symptoms compared with clinicians. The findings are presented below.
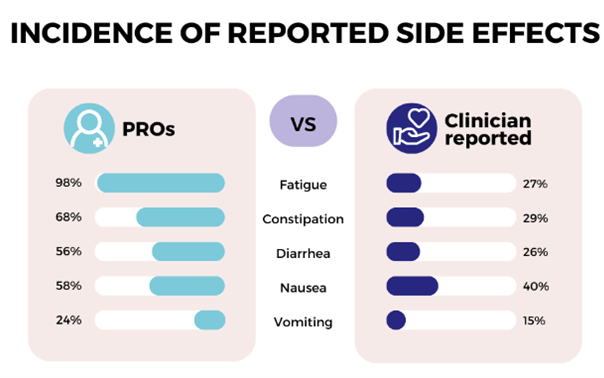
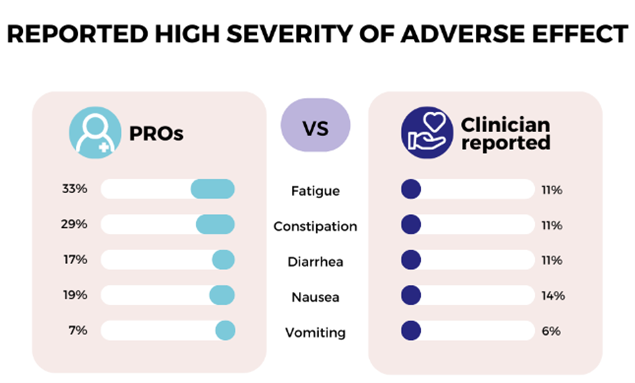
Although different scales were used, the differences in symptom rates reported by patients and clinicians were clinically meaningful. This information may have an impact when managing symptoms, including evaluations by clinicians and the communication of symptom expectations for patients.
PROs should be incorporated into studies alongside standard adverse events to better represent the patient experience.
Source: Thompson CA, Mehta-Shah N, Flowers C et al. Patient- versus clinician-reported symptoms in the POLARIX study. Presented at ASCO 2023 (2–6 June; Chicago, IL, USA).